By Michael Mozdy
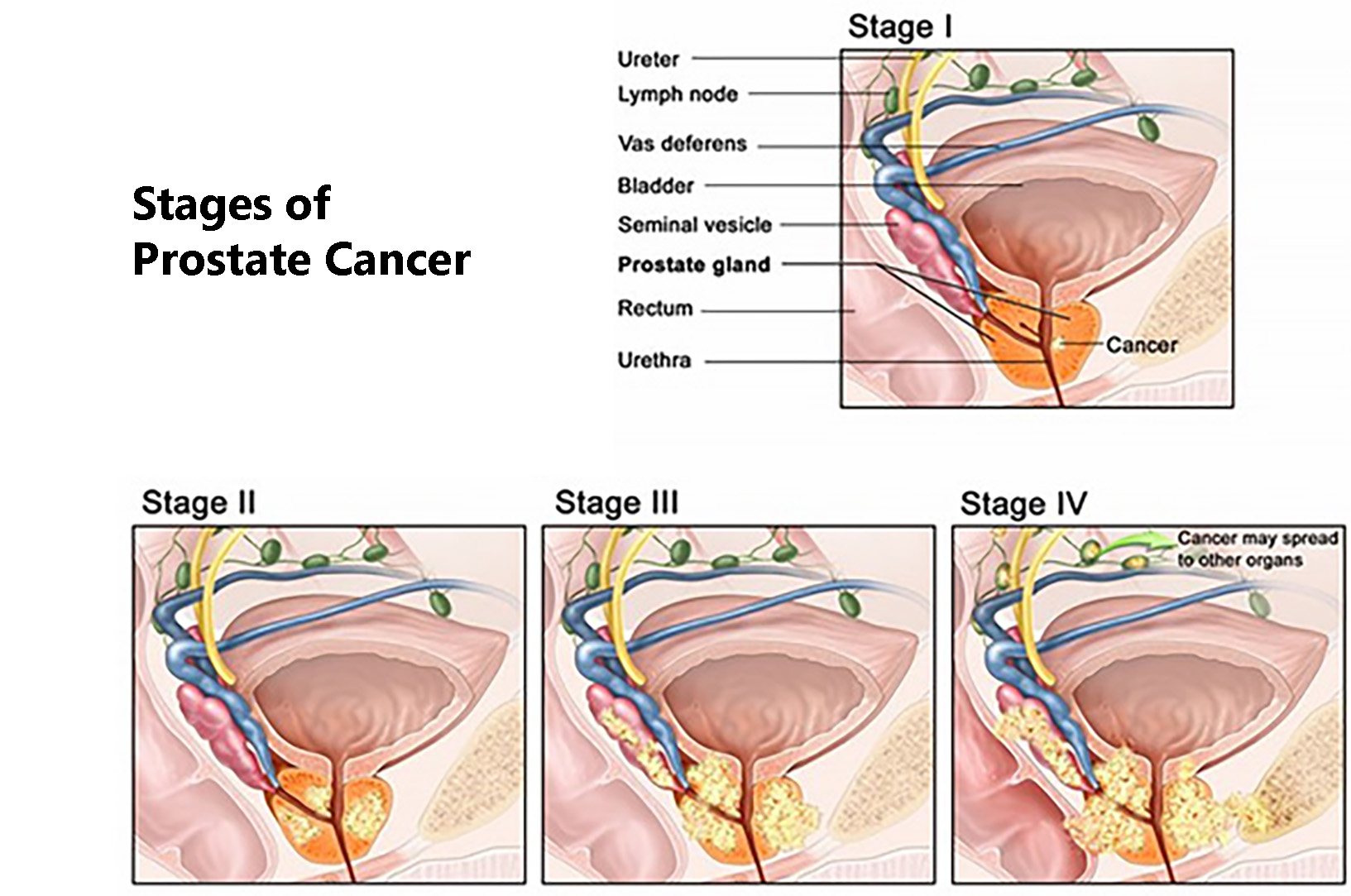 If you’re a man over the age of 50, chances are you’re a little concerned about prostate cancer. After all, it’s the most common solid tumor cancer for men, and 1 in 7 men in the U.S. will have it in their lifetime.
If you’re a man over the age of 50, chances are you’re a little concerned about prostate cancer. After all, it’s the most common solid tumor cancer for men, and 1 in 7 men in the U.S. will have it in their lifetime.
Urologists combine several data points to assess a man’s risk for cancer: a digital rectal exam, a PSA blood test, and family history, to name some of the most important. If there is a concern, urologists perform a biopsy to determine if there is any cancer. Until now, biopsies have involved a fair amount of guesswork.
The traditional “first line” procedure is called transrectal ultrasound (TRUS) guided biopsy. It can be done fairly easily in an office setting, although with some discomfort for the patient. With the aid of an ultrasound probe to locate the prostate, the urologist will take about 12 core needle biopsies from different parts of the prostate. Why so many? The prostate is a small gland in the center of the pelvis, and ultrasound doesn’t have great resolution for soft tissue, so it cannot reliably detect areas of concern. Thus, even with ultrasound guidance, TRUS prostate biopsies use 12 core needle samples to increase the likelihood of getting a sample of concerning tissue.
It’s a far cry from being accurate. While TRUS biopsies find cancer 44% of the time,1 studies have shown that there’s up to a 30% chance of a false negative.2 In other words, 30% of the time when a biopsy is negative, cancer actually exists in the prostate, but the method is too flawed to find it.
As a contrast, it's certainly not the procedure used for breast biopsy, where mammography provides much better location information for where to take the biopsy. The location and size of the prostate makes traditional biopsy much more of a random sample.
Interventional radiologist Claire Kaufman and abdominal radiologists Jeffrey Olpin, MD, and Glen Morrell, MD, PhD are three of a handful of physicians in the country providing a better approach: real-time MRI-guided prostate biopsy.



Claire Kaufman, MD, Jeffrey Olpin, MD, and Glen Morrell, MD, PhD.
If concerned about cancer, some urologists today order an MRI scan as a reference guide for their biopsies. MRI is more expensive than other scans like ultrasound, but it provides a detailed look at the prostate and is far superior at detecting areas of concern. This scan is done in advance, often weeks or even months before the biopsy, and it exists as a prior study on a computer screen. Since many prostate tumors measure just 5-6mm wide, trying to biopsy the tumor with 12 core needle samples and a computer image is still a proverbial (and literal) shot in the dark.
This is where interventional radiology comes into play. The detailed and sophisticated imaging provided by MRI has been helpful in the diagnosis of countless diseases, but using it in an intervention – like a biopsy – has been a trickier proposition. First, the MRI machine contains a large, powerful magnet, so specialized, non-magnetic instruments are needed. Second, reading MRI scans takes a great deal of training (prostate scans are particularly difficult to read), and so most non-radiologists are not trained to use the MRI information to help guide a procedure. A radiologist with both the training to read the scans and the ability to perform biopsies is the person to accomplish the task.
For these reasons, MRI-guided prostate biopsies are not easy to come by. Here in Utah, there’s one place with the equipment: University of Utah Hospital. San Francisco and Oregon Health & Science University are the closest places outside of the state where patients can get one done.
In the 30-minute procedure, the patient is given conscious sedation, and placed inside an MRI machine. Kaufman, Olpin, or Morrell positions a non-magnetic titanium needle with the help of very specific MRI scans. When satisfied with the exact positioning, our radiologist takes three to four biopsies with the push of a spring-loaded trigger.
 |
| The device used for real-time MRI-guided prostate biopsies and the MRI images used during the procedure |
Note that this technique is different from what some physicians are calling the "fusion" method of MRI-targeted prostate biopsy where they overlay a previously done prostate MRI with real-time ultrasound data, thanks to some sophisticated software. While this fusion procedure is convenient for a urologist to perform in his or her office, Kaufman points out that the error in the resolution of this method is around 3-4 mm, which is close to the size some tumors can be.
University of Utah urologists Will Lowrance, MD, MPH, and Chris Dechet, MD, lobbied the hospital and the radiology department to invest in the equipment and skills to perform real-time MRI-guided biopsies. “We have used prostate MRI in the treatment planning phase of managing prostate cancer for many years,” explains Lowrance. “Because of the high quality of our prostate MR images, it is only natural that its use would begin to migrate into the screening/diagnostic phase of prostate cancer.”
Lowrance and Dechet first thought that they’d use this procedure with only a few patients they were very concerned about where traditional biopsies weren’t revealing cancer – about two or three patients a year. In the first year, however, we performed 43 biopsies in 35 men – about three to four a month.
 |
| Urologists Will Lowrance, MD, MPH (left), and Chris Dechet, MD |
Lowrance is enthusiastic about this technique’s usefulness. “It has been very helpful in how we manage men with an elevated PSA that have undergo a negative standard prostate biopsy in the past,” he says. “It certainly helps us to a better job of diagnosing men with prostate cancer located in the front (or anterior) portion of their gland.”
The type of procedure used by Kaufman, Olpin, and Morrell is, in fact, much better than the traditional TRUS biopsies. Because of lower costs, a shorter time commitment, ease of accessibility, and known outcomes as a screening tool, the TRUS biopsy done at a urologist’s office is still the recommended first line procedure. But if these biopsies are negative and the urologist is still concerned about cancer, MRI-guided biopsies are the next step to see if cancer can be detected. Studies have shown that our technique of real-time MRI guided prostate biopsy can find cancer in up to 59%3 of patients who have already had at least one negative TRUS biopsy.
This is a somewhat stunning success rate, considering that these patients already had a negative biopsy. The American Urology Association was so impressed by these results that they've issued a new recommendation that MRI-guided biopsy be the second-line procedure for cancer detection. Kaufman, Olpin, and Morrell expect that these imaging-guided procedures will become more and more common as health care systems make the investment to offer them.
Thirty-five patients had the procedure in 2016. Some of these men have had up to six biopsies over the years - all negative - but this procedure reveals cancer because of the accuracy of the technique in retrieving the correct biopsy sample. You can just imagine their relief over finally having a definitive diagnosis.
The only other cancer care pathway using MRI-guided biopsies is breast cancer, and the mammographers at the Huntsman Cancer Institute perform about 1-2 of these per week. Kaufman, Olpin, Lowrance, and Dechet are glad to be able to provide this same level of service and accuracy for prostate cancer.
__
The American Cancer Society estimates that in 2017, there will be 161,360 new cases of prostate cancer that are diagnosed. They estimate that 26,730 men will die from prostate cancer in 2017 as well. Thankfully, the 5-year survival rate for prostate cancer that is either local or regional (i.e., has not metastasized far beyond the prostate) is nearly 100%. This makes detection of prostate cancer before it may metastasize an important goal.
1 Presti JC, Jr., O'Dowd GJ, Miller MC, et al. Extended peripheral zone biopsy schemes increase cancer detection rates and minimize variance in prostate specific antigen and age related cancer rates: results of a community multi-practice study. J Urol . 2003;169:125-129.
2 Serefoglu EC, Altinova S, Ugras NS, Akincioglu E, Asil E, Balbay MD. How reliable is 12-core prostate biopsy procedure in the detection of prostate cancer? Canadian Urological Association Journal. 2013;7(5-6):E293-E298. doi:10.5489/cuaj.11224.
3 Hambrock T, Somford DM, Hoeks C, Bouwense SA, Huisman H, Yakar D, van Oort IM, Witjes JA, Fütterer JJ, Barentsz JO. Magnetic resonance imaging guided prostate biopsy in men with repeat negative biopsies and increased prostate specific antigen. The Journal of urology. 2010;183(2):520-8.
__
This story was updated in October, 2019