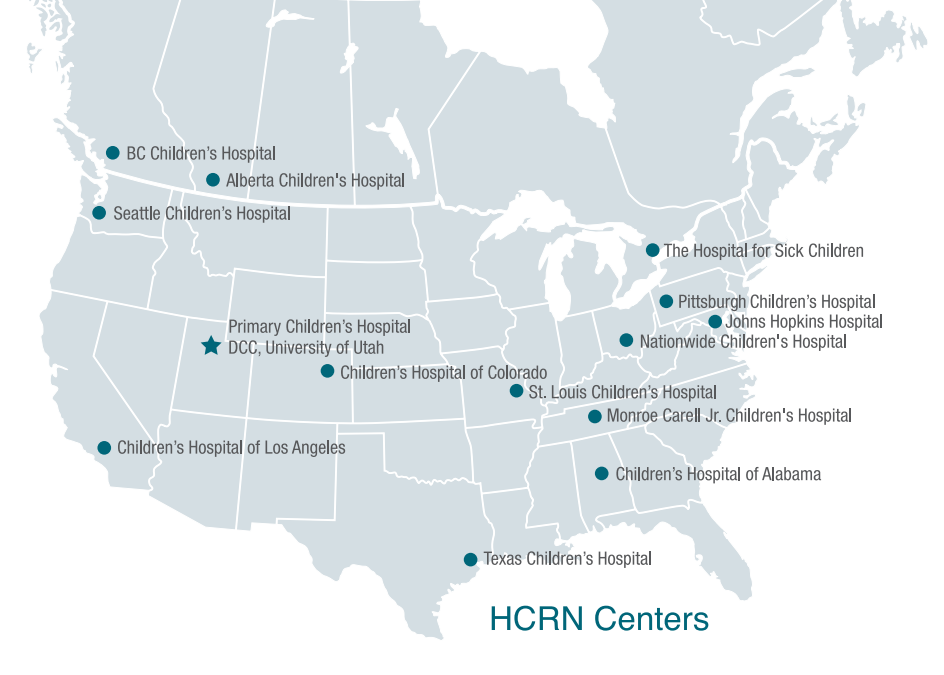
In 2006, John Kestle, MD, started the Hydrocephalus Clinical Research Network (HCRN) to promote collaboration between providers and find new solutions to help children with hydrocephalus. The goal of the network is to explore ways to treat patients that will lead to longer, less difficult lives than is possible at present.
The current prevailing treatment method, shunting excess cerebrospinal fluid to another location in the body, works well and improves lives, but it does come with some drawbacks that Kestle and the rest of the HCRN want to resolve, whether through innovation or updates to current methods. Shunt use began in the 1940s, rose in popularity through the 60s, and continues today. Unfortunately, shunts are often prohibitively expensive, costing thousands of dollars. There is also a significant risk of infection that comes with implanting foreign substances in the body; shunts are life-time implants that can be difficult to manage both for parents and for patients as they age. And, probably most influential in the pursuit of new treatment methods: a shunt will nearly always fail. In fact, 40–50% fail within 2 years of placement, and 80–90% fail within 10 years. On average, shunts will malfunction 2–3 times and require multiple operations over the course of a patient’s life.
In the early 2000s, Benjamin Warf, MD, was working on hydrocephalus cases in Uganda and became concerned about treating children with shunts in rural areas where access to care is not guaranteed. He knew that children who experienced shunt failure might die before reaching a clinic that could address the failure, so he began looking for other treatment solutions.

Dr. Warf decided to combine two well-known procedures to treat hydrocephalus in a novel way: endoscopic third ventriculostomy (in which an opening is created in the floor of the third ventricle to allow cerebrospinal fluid to drain) and choroid plexus cauterization (which decreases the amount of cerebrospinal fluid produced). The combination of these two procedures (known as ETV+CPC) allows patients to avoid the excessive cost of shunt placement and is associated with lower risk, especially as patients age. This method has now been used to treat many children (approximately 800 infants per year) in Uganda and surrounding countries.
While it’s incredible to see a new treatment method develop in a low-income country and then spread to the rest of the world, these methods cannot be immediately applied in the United States because most cases of hydrocephalus in Uganda stem from infection from meningitis whereas most cases in the US are congenital. It is also unclear whether the cognitive outcome of patients after ETV+CPC is equivalent to that of patients who have had a shunt placed.

Therefore, in 2019, Dr. Kestle applied for and received an almost $10 million grant to continue studying hydrocephalus with the HCRN and to perform a trial based on the research done by Dr. Warf in Uganda. The primary questions Dr. Kestle hopes to answer during the course of the trial are 1) do the results seen by Dr. Warf translate to a patient population with congenital hydrocephalus rather than post-infection hydrocephalus, 2) will the enlarged ventricles (which studies show do not shrink after ETV+CPC) cause problems as the child grows, and 3) as patients age and are more removed from the initial surgery, will they continue to see outcomes as good as or better than the outcomes seen with shunting over the past 80 years?
The trial runs from September 2019 through August 2027 and is approximately halfway through accrual. Patients are monitored for up to 5 years (with a 1-year minimum follow-up) after their first treatment for hydrocephalus. Although the trial is not complete and outcomes are still being determined, we’re proud to have Dr. Kestle at the forefront of this research in the US and excited to see the progression of this work as patients age and it can be determined whether the long-term outcomes of this surgery will be better than those of shunting.