Welcome to the Affiliated Projects page!
To have your project(s) added, contact us @parcka@hsc.utah.edu
Jake Magel, PT, PHD, DSc, FAAOMPT
PT-IN-MIND
Study Overview
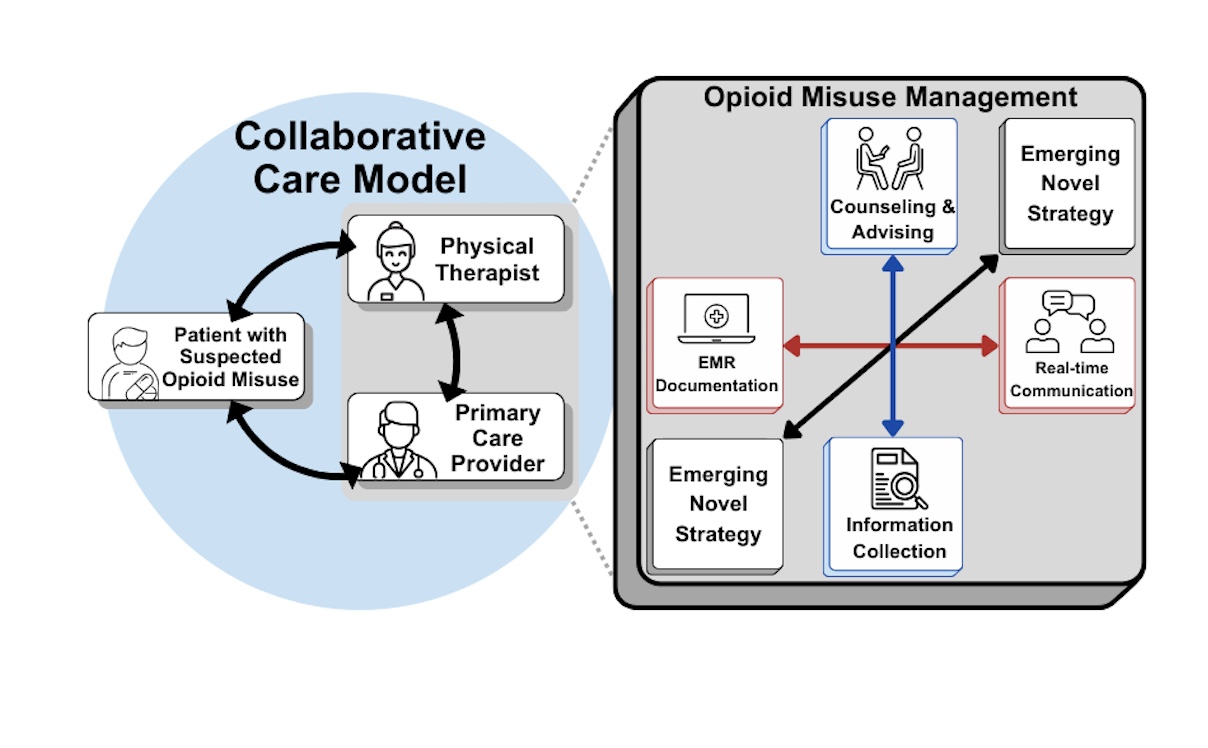
Most patients treated by outpatient physical therapists (PTs) have musculoskeletal pain and 1 in 3 use prescription opioids. About 25% of those with musculoskeletal pain who are prescribed opioids for 90 or more days may have opioid misuse (taking prescription opioids in ways other than prescribed). PTs, Primary Care Providers (PCP), addiction leaders and scholars advocate that PTs should play a greater role in screening and addressing patients with opioid misuse. Unknown are the PCPs attitudes toward PTs’ role, competency, and adequacy in addressing opioid misuse, the PCPs preferences for how PTs should screen and address opioid misuse and the strategies for PTs to communicate with PCPs about patients with suspected opioid misuse. PCPs coordinate and prescribe opioids for patients. Although unknown, PCPs may not favor PTs in identifying and/or addressing opioid misuse among their patients; strategies for how to communicate this condition in a collaborative way may improve communication between PTs and PCPs about opioid misuse.
Study Aims:
Aim 1: Evaluate the attitudes of PCPs toward PTs (e.g., PTs’ adequacy and legitimacy in their role), addressing opioid misuse in outpatient physical therapy practice. We will use surveys and semi-structured interviews to understand PCPs attitudes toward PTs addressing opioid misuse.
Aim 2: Determine the optimal strategies for PTs to work collaboratively with PCPs about patients with suspected opioid misuse. Semi-structured interviews with PCPs will be used to understand the optimal strategies for PTs to work collaboratively with PCPs to address opioid misuse.
Aim 3: Develop a treatment manual for PTs to address and communicate opioid misuse using the results from Aims 1 and 2. We will develop an initial draft of a treatment manual followed by checking the manual with PCPs then finalize the manual. Our results will provide pilot data to test the effectiveness of PTs to address opioid misuse.
PT PCP Attitudes
Background
Our project will determine PCP preferences for collaboration strategies from PTs and will advance our ongoing program to develop PT-led interventions to address patients with long-term opioid treatment and suspected opioid misuse (S-OM). Our program of research examines, and aims to improve, clinical outcomes by addressing opioid misuse and preventing the transition to OUD and potential overdose. Our work in opioid misuse communication and collaboration will also be applicable to communication and collaboration from PTs to PCPs regarding other vulnerable conditions (e.g., suicidality, physical or mental harms). Our work is grounded in the collaborative care model,21 a systematic approach to effectively manage chronic conditions (e.g., opioid misuse, pain) through integration of PTs and other providers (PCPs).
Our long-term goal is to improve outcomes of patients with opioid misuse and co-occurring musculoskeletal pain who are managed by PTs.
Our objective for this proposal is to understand the optimal means to promote collaboration between PTs and PCPs for patients with opioid misuse.
Study Aims:
Aim 1: Understand the role of the PT from the PCP perspective and preferred collaborative strategies for patients with S-OM. Our mixed-methods approach entails sequential collection and qualitative data analysis to (1) explore PCP perceptions about whether PTs should screen, refer, or counsel patients with S-OM; (2) how PTs should communicate S-OM to a PCP; and (3) understand the next steps a PT should take to address a patient with S-OM using 20 semi-structured interviews, followed by quantitative survey data to confirm these perceptions and strategies in a larger cohort of PCPs.
Aim 2: Evaluate PCP attitudes and beliefs about PTs adequacy and legitimacy in screening, referring, and counselling patients for S-OM. Our approach will survey PCPs using a modified version of the Drug and Drug Problems Perception Questionnaire Role (DDPPQ) Adequacy and Role legitimacy subscales.
Aim 3: Develop a training manual for PTs to work collaboratively with PCPs to manage S-OM among patients. An iterative approach for manual development will include 1) incorporating Aims 1 and 2 results and our research team expertise to develop an initial draft and 2) recruiting PCPs who participated in Aim 1 interviews to review and amend the manual for final draft.
Opioid Misuse Training Program
Background
The U.S. Preventive Services Task Force7, stakeholders, and addiction scholars8 and have called for all healthcare providers to be trained to screen, assess, treat or refer patients who engage in drug use. PT leaders, including members of our research team, advocate for physical therapists to play a greater role screening and managing patients with OM.9 As such, our research team conducted a national survey of physical therapists about their readiness to manage patients with orthopaedic conditions and co-occurring OM. More than 89% of respondents agreed that physical therapists can play a role in modifying patterns of opioid use.10 Preliminary results of our ongoing survey of patients seen in PT (n=869) indicates that if a physical therapist suspects OM, 81% of patients agree that the physical therapist should engage the patient in a conversation about OM and 87% of patients agree that it is appropriate for the physical therapist to refer the patient to a specialist to address OM. Leveraging the PT setting to engage patients with OM could mitigate the transition to OUD and prevent opioid-related overdose and death.
Our long-term goal is to improve the management of patients with OM in the PT setting. Developing procedures that physical therapists can easily implement into routine clinical practice for patients who may have OM is a critical first step.
The purpose of this study is to develop and operationalize key procedures for physical therapists (n = 12) to address patients who are at risk for or have OM. We will train physical therapists in procedures to:
1) Engage patients at risk for OM in conversations about appropriate opioid use
2) Screen
3) Assess these patients for OM
4) Refer patients for further treatment if OM is suspected
Study Aims:
1. Qualitatively evaluate physical therapists' perceptions and recommendations for implementing OM procedures. Our approach will be to conduct 1 focus group composed of the physical therapists who attended the training after presenting each session for a total of 2 focus groups (i.e., 1 focus group each for engaging patients in conversations about opioid use, screening and assessing patients for OM and referring patients for further treatment of OM) to evaluate the physical therapists’ receptivity to the procedures. During these focus groups, a modified Delphi methodology will be used to arrive at final operationalized procedures, which will be manualized.
2. Evaluate the implementation of the manualized OM procedures. We will use the RE-AIM framework to guide our evaluation of Aim 2. Our approach will be to use mixed-methods to quantitatively assess key implementation measures including but not limited to the proportion of physical therapists that agreed to attend the training that completed the training, OM knowledge and attitudes test scores pre- and post-training testing, the number physical therapist who screened, assessed and referred a patient with OM for further treatment. Next, semi-structured interviews will be used to provide context to our quantitative results and to assess barriers and facilitators to the implementation of the OM procedures.
Elizabeth Siantz, PhD, MSW
Adapting and Implementing a Chronic Disease Self-Management Program for persons with opioid use disorders and serious mental illness
Study Overview
People with opioid use disorder (OUD) have a high co-occurrence of serious mental illness (SMI) and other chronic diseases, and are often challenged by their clinical symptoms and social vulnerabilities. While primary care settings frequently treat patients with OUD and SMI, primary care providers have few tools to support this population in self-managing these complex health conditions. The Chronic Disease Self-Management programs (CDSMP) can improve disease management skills and behaviors of people with chronic diseases but have not been adapted for primary care patients with OUD and SMI. Un-adapted versions might lack relevance to this population and setting. In this research project, Dr. Siantz will address this implementation gap through the following specific aims
Aim 1: Adapt the CDSMP for adults with OUD, SMI, and chronic disease for implementation in primary care settings using the CIPF. With my mentors, I will develop a Community Advisory Board (CAB). We will collaboratively adapt the CDSMP to improve relevance for this population and setting by exploring contextual factors that impact program implementation. This Research Aim corresponds with my Career Aim 1: develop expertise in intervention adaptation especially as it relates to the OUD population and associated mental health and primary care needs.
Aim 2: Test the feasibility, acceptability, and initial impact of adapted CDSMP for persons with SMI and OUD in a primary care setting. I will randomize patients at two primary care sites to receive adapted CDSMP or primary care treatment as usual, study feasibility (e.g., program attendance), acceptability (e.g., participant satisfaction), and initial outcomes (e.g., patient activation). This Aim corresponds with my Career Aim 2: ac-quire training in clinical trial design and management in real-world settings.
Aim 3: Evaluate implementation process and context of the adapted CDSMP using RAPICE. I will conduct interviews with study participants and clinic staff to understand how the CDSMP compares to usual care, implementation barriers and facilitators, and how study site differences impacted implementation. This research Aim corresponds to my Career Aim 3: obtain advanced skills in intervention implementation qualitative evaluation methods, particularly the RAPICE method.
Our Team
Principal Investigator: Elizabeth Siantz, PhD, MSW
K01 Mentoring Team: Adam Gordan, MD, MPH (Primary Mentor); Leopoldo Cabassa, MSW. PhD (co-mentor)
K01 Advisory: Angela Fagerline, PhD; Gerald Cochran, MSW, PhD; Lawrence Palinkas, PhD
Research Assistant: Emily Rougelot, MSW candidate