Pediatric Research

Pediatric Research
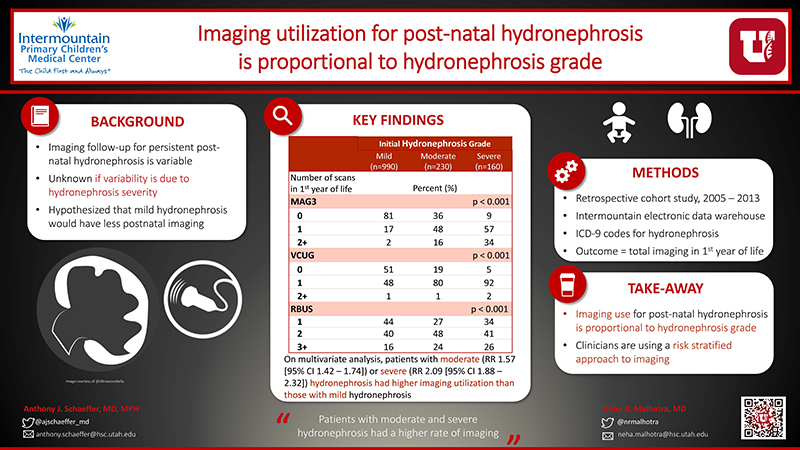
Frequency of imaging in infants with uretero-pelvic junction-like hydronephrosis
Anthony J. Schaeffer, MD, MPH, Neha R. Malhotra, MD, Glen A. Lau, MD, Patrick C. Cartwright, MD, Nora F. Fino, MS, Flory L. Nkoy, MD, MS, MPH, Mark D. Ebert, MD, Rachel Hess, MD, MS
University of Utah, Salt Lake City, UT, USA
READ THE ABSTRACT
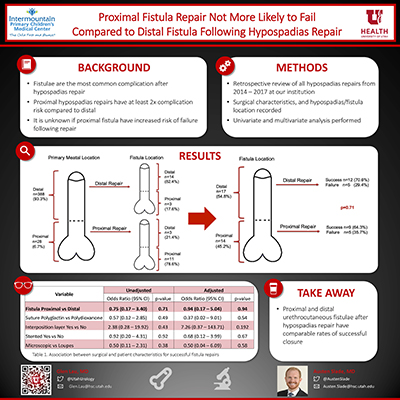
Closure of distal versus proximal urethrocutaneous fistulae after hypospadias repair
Austen D. Slade M.D., Neha M. Malhotra M.D., Anthony J. Schaeffer M.D., Patrick C. Cartwright M.D., Glen A. Lau M.D.
Salt Lake City, UT
Objectives
Urethrocutaneous fistulae are the most common complication following hypospadias repair, and proximal hypospadias carry a nearly two-fold risk for fistula formation compared to distal. The impact of fistula location on success of repair has not been well studied. We hypothesized that repairs of distal fistulas would be more successful when compared to proximal fistulas and aimed to identify surgical factors that may affect these outcomes.
Methods
Retrospective review of all patients undergoing repair of fistula at our institution from 2014 to 2017 following hypospadias repair. Data collected included location of fistula, size of fistula, type of magnification used, suture type, use of post-operative stent, number and type of interposition layers used. Univariate analysis was performed using chi-square tests for categorical variables, multivariate analysis was performed using logistic regression.
Results
During the study period 31 patients presented for fistula repair. There were 17 (54.8%) distal and 14 (45.2%) proximal fistulas. There was no difference in success for distal (70.6% successful) vs proximal (63.4%) fistula repair (p = 0.71). Proximal fistulae were not more likely to be stented (p=0.24) but were more likely to have had an interposition layer (p=0.02). Median age at initial repair was 7 months (IQR 5, mean 11.5 months). Median time from hypospadias repair to diagnosis of fistula was 7 months (IQR 11.5, mean 9.8 months).
Conclusions
Based on our data, proximal and distal fistulae after hypospadias repair have comparable rates of successful closure. Notably, proximal fistula repairs were more likely to utilize an interposition coverage layer than distal fistula repairs. Use of an interposition layer has previously been shown to decrease fistula formation after initial hypospadias repair, and this could also affect outcomes in fistula repair.
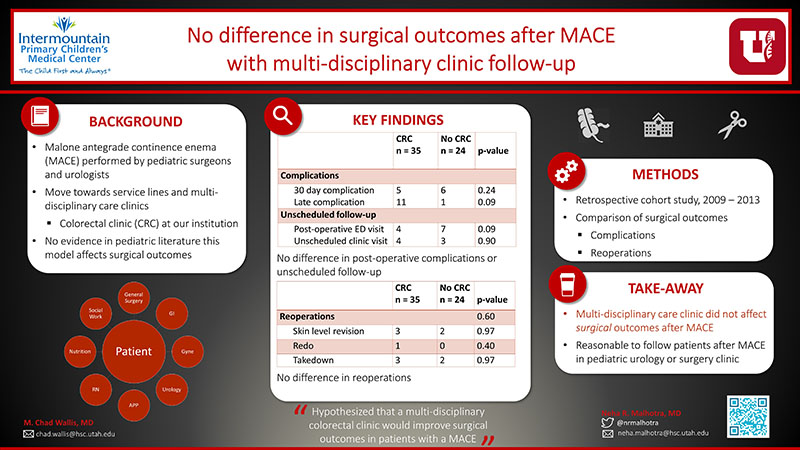
The effect of a multidisciplinary colorectal clinic on Malone antegrade continence enema (MACE) outcomes
Neha R. Malhotra, Glen A. Lau, Austen D. Slade, Zachary J. Kastenberg, Sarah Zobell, Michael D. Rollins, M. Chad Wallis
1University of Utah, Department of Surgery, Division of Urology
2University of Utah, Department of Surgery, Division of Pediatric Surgery
Introduction
The Malone antegrade continence enema (MACE) allows patients to perform colonic irrigation, manage fecal incontinence and empty in a more predictable manner, improve social continence. Various technical modifications have improved outcomes and decreased complications. A critical component to success is regular follow-up and adherence to a bowel program; therefore, it has been suggested that a team approach to bowel management should be employed. We hypothesized that a multi-disciplinary colorectal clinic would improve surgical outcomes in patients with MACE.
Materials and Methods
A multi-disciplinary colorectal clinic (CRC) was implemented at our institution in 2011. This clinic, led by a general surgeon, is a collaborative effort between general surgeons, urologists, gastroenterologists and gynecologists and utilizes physicians, advanced practice providers and nurses as well as social workers and nutritionists. All patients undergoing MACE are eligible to follow in CRC, regardless of operating service. Patients undergoing MACE in the two years prior (2009, 2010) and the two years after (2011, 2012) were identified and a retrospective chart review was performed. Outcomes of patients who were followed in CRC were compared to those who did not follow in CRC (control group). Univariate analysis was performed using chi-square tests for categorical variables. A small sample size precluded multivariate analysis. Mann-Whitney test was used to analyze non-parametric variables. Statistical significance was determined by a p value of < 0.05. Statistical analysis was performed using SPSS Version 25 (IBM, Armonk, NY).
Results
59 patients were identified in the four years prior to and after initiation of CRC; 35 (59.3%) patients were followed in CRC and 24 (40.7%) were not. Patients in CRC were more likely to have phone appointments (CRC median 3, control median 0; p =<0.01), but had comparable numbers of clinic visits (CRC median 4, control median 6; p = 0.17). There was no difference in post-operative ED visits (p = 0.09), unscheduled post-operative clinic visits (p = .90), early complications (p = 0.24), late complications (p = 0.93), or reoperations (p = .60; skin level revision p = 0.97, takedown p = 0.97, re-do MACE p = 0.40) in either cohort. Patients undergoing MACE by general surgery were more likely to be seen in the CRC than urology patients (14.3% of urology MACEs, 76.7% of general surgery MACEs; p < 0.01)
Conclusion
Our study did not show a difference in surgical outcomes with follow-up in a multidisciplinary colorectal clinic; this may have been due to limited sample size. Our results do show a significant increase in phone visits and a non-significant decrease in clinic visits. There was no difference in post-operative ED visits, patient phone calls or unscheduled visits. Further work is necessary to determine if increased phone follow-up with potentially decreased clinic visits improves patient satisfaction and decreases cost of care.
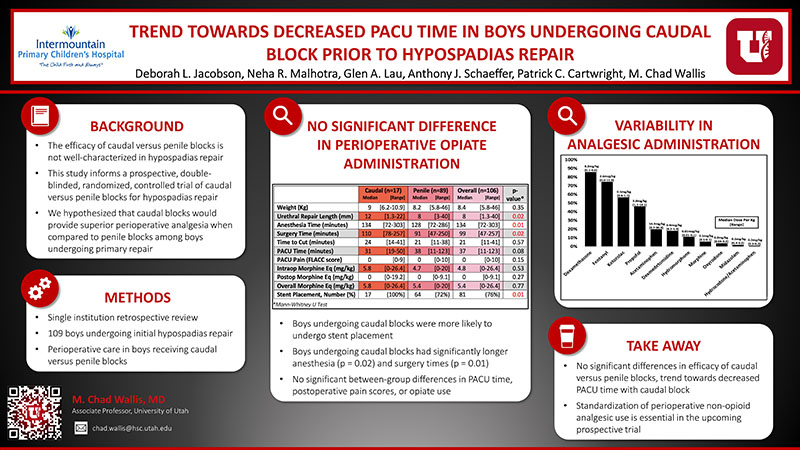
Efficacy of Caudal Versus Penile Blocks in Hypospadias Repair
Deborah L. Jacobson, Neha R. Malhotra, Glen A. Lau, Anthony J. Schaeffer, Patrick C. Cartwright, M. Chad Wallis
Purpose
The efficacy of caudal versus penile blocks is not well characterized among boys undergoing hypospadias repair. This study informs a prospective, double-blinded, randomized, controlled trial of caudal vs. penile blocks for hypospadias repair. We hypothesized that caudal blocks would provide superior perioperative analgesia.
Methods
A single-institution retrospective review of prospectively-enrolled boys undergoing initial hypospadias repair was performed. Boys were excluded if they received dual caudal and penile blocks, if electronic anesthesia records were not available, or if additional procedures were performed under the same anesthetic. Patient characteristics, procedure characteristics, postoperative times, pain scores in the first 2 postoperative hours, and opioid administration were recorded. Univariate, non-parametric tests of significance were performed to evaluate between-group differences.
Results
106 boys were repaired at a median 7.3 months. The median urethroplasty length was 8mm and 76% of repairs were stented. 89 boys received penile blocks and 17 received caudal blocks. The groups were similar in terms of age and weight. The group receiving caudal blocks had a significantly longer urethroplasty length (p = 0.02; Table 1). The median anesthesia and PACU times were 134 and 37 minutes, respectively. The median intra- and postoperative weight-based morphine equivalents administered were 4.8mg/kg and 0mg/kg, respectively. Boys undergoing caudal blocks were more likely undergo stent placement and had significantly longer anesthesia (p = 0.02) and surgery (p = 0.01) times. There were no significant between-group differences in PACU time, postoperative pain scores, or opioid use. Perioperative use of non-opioid analgesics was variable (Table 2).
Conclusions
While no significant differences in the efficacy of caudal versus penile blocks were demonstrated, there was a trend towards decreased PACU time in boys undergoing caudal blocks. Standardization of perioperative non-opioid analgesic use is essential in the upcoming prospective trial.