RAIN Background
As the US is confronted with a rise in opioid use disorder (OUD), opioid misuse, and opioid-associated harms, opioid-related overdose deaths more than quadrupled from 1999 to 2016. As of 2019, 9.7 million Americans reported using prescription opioids non-medically. Opioid-related overdose fatalities had an economic cost of more than $75 billion for the US in 2016. The scarcity of prevention and treatment services for addiction in rural areas necessitates a broad-based health system response. New, sustainable interventions to educate the healthcare workforce about substance use disorder(SUD)/OUD and training for implementation of evidence-based strategies in rural areas to confront emerging SUD/OUD are urgently needed.

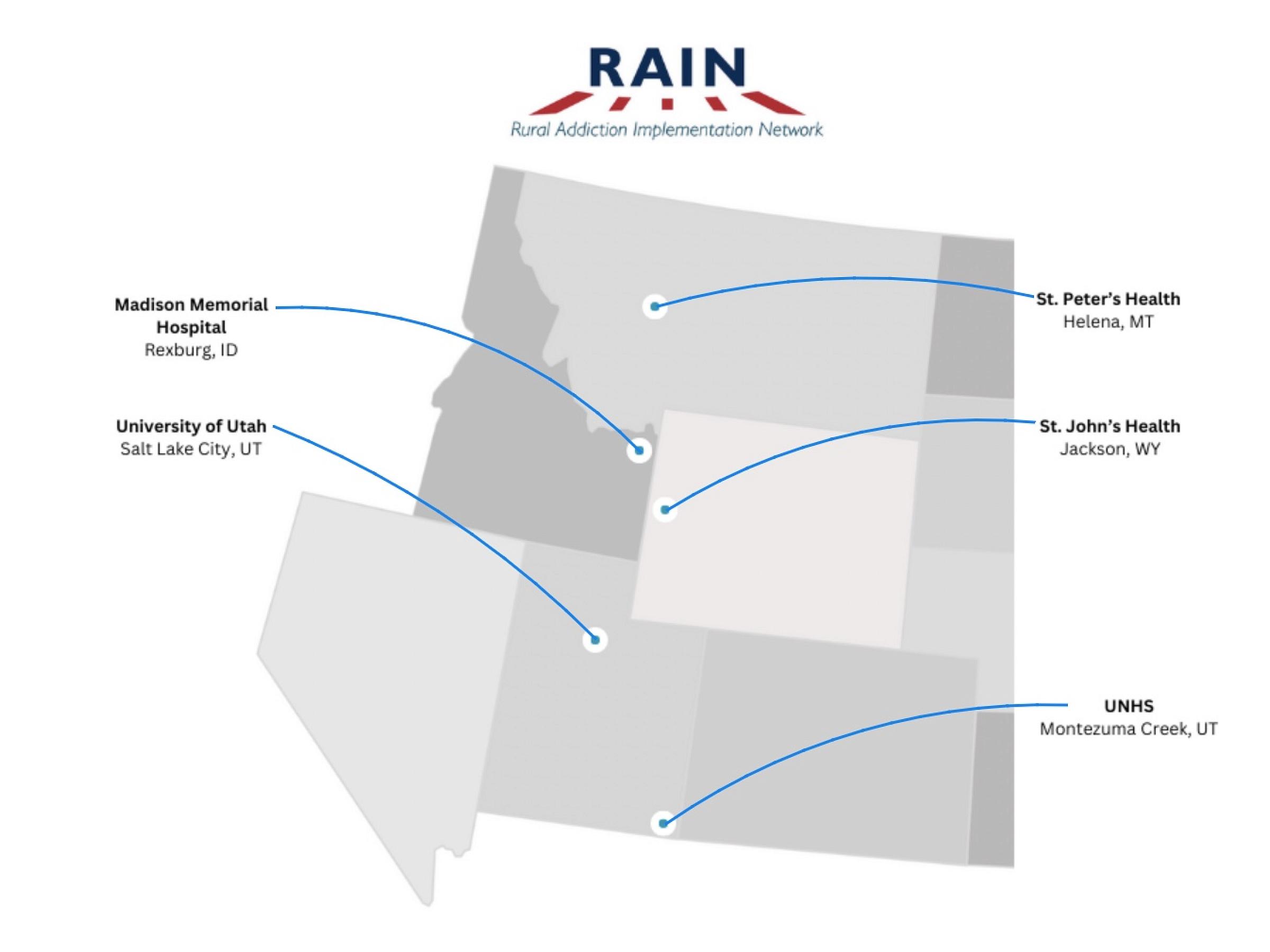
Our rural environments here in Utah, Wyoming, Idaho, and Montana, like many rural communities across the US, have been disproportionally impacted by opioids. We are seeing overdose rates and rates of OUD diagnosis higher in rural communities compared to urban communities and SUDs are more harmful in rural areas. Unfortunately, rural counties are more than twice as likely to have opioid overdoses with most counties severely lacking treatment capacity for SUD/OUD. OUD treatments are traditionally located in urban environments, therefore there is an urgent need to be innovative in addressing addiction engagement in rural areas.
Research at the University of Utah and other academic centers have shown OUD can be effectively identified and treated in non-addiction specialty health care settings, such as primary care, hospital-based settings, and rural hospital network settings. However, there are challenges in implementation of evidence-based addiction practices into real-world practice making it difficult to handle addiction treatment in our rural communities. Addiction care is hindered by the low quality of its treatment infrastructure, and lack of addiction education among healthcare professionals. Educating rural health care providers about 1) SUD/OUD prevention, treatment, and recovery and 2) training for implementation of these practices, has the dual opportunity to develop a sustainable infrastructure where new evidence-based addiction practices can be rapidly and effectively implemented over time in rural healthcare settings.
Madison Memorial Hospital
- Current efforts are focused around continuing the post-partum support group and implementing Keepin' It Real for the Fall 2024 school year.
St. Peter's Health
- The Licensed Addiction Counselor at St. Peter's has earned a Level 1 certification in the Invitation to Change (ITC) Approach. This certification, awarded by the CMC: Foundation for Change, demonstrates advanced expertise in ITC and authorizes the counselor to lead ITC community groups.
Utah Navajo Health System (UNHS)
- A new law, known as SB26 Behavioral Health Licensing Amendments, was enacted to address the shortage of licensed therapists on Utah's tribal lands. It allows prospective therapists who do not pass the national licensure exam to meet other requirements instead, making it easier for Native Americans to become licensed therapists and serve their communities.
St. John's Health
-
The internal addiction management group at St. John's continues to develop new patient referral pathways, improving addiction treatment and the continuum of care.
Madison Memorial Hospital
Accomplishments with RAIN
- Hire a BYUI Intern- To collaborate and help in communication between RAIN and Madison Memorial.
- Take Back Program- Was established with help from local police department and community efforts.
- K-12 Education Program- Rexburg implemented the Botvin Training into 7th grade health classes in the 22-23 school year. Follow-up qualitative interviews with teachers will be done once the school year has finished.
- Outpatient Mental Health- Madison Memorial has identified a need to have an outpatient mental health service for the community.
- Postpartum Social Workers- Implement and fund two community social workers to conduct substance use group sessions for postpartum women.
- Meds to Beds- Implement a possible pilot system in Impatient to have medication instructions sent bedside from the pharmacy. Most likely a narcotic specific system.
- Risk Screening in EMR- Attempting to implement a system in place at the University of Utah for risk screening, possibly according to CMS standards.
- Behavioral Health Crisis Intervention Instructors Certificate- Madison wants to certify two individuals to be instructors for non-violent crisis intervention with advanced physical skill. These two individuals will then host monthly trainings for staff.
- ER Bridge Program- Train 3 social workers to be patient navigators, helping patients from the ER to primary care or other resources.

St. Peter's Health
Accomplishments with RAIN
- Naltrexone and Sublocade Initiation- Pharmacy to request formulary in hospital pharmacy for Naltrexone and Sublocade.
- Narcan/Suboxone "to go" kits for ER- Kits provided from the ER with instructions for use. State can supply Narcan and it would be beneficial to have excess available.
- SUD Training by MPC- Montana Primary Care has been funded to train St. Peter's hospital staff on SUD/Stigma.
- OUD Team Collaboration and Training- Provide addiction clinic/ER staff a team building opportunity to attend ASAM or other conference.
- Coordinate with County Jail- Interact with County Jail to obtain information on treatment provided and discharge guidance.
- UDS Improvement Program- Current UDS kits are poor in scope and slow in evaluation time. Searching for an alternative like through millennial health.
- SUD Coordination and Discharge- Discharge from in-patient units to outpatient addiction or behavioral health services to better coordination.
- LAC- A Licensed Addiction Counselor was hired and will soon be leading community groups with the Invitation to Change (ITC) Approach.

UNHS
Accomplishments with RAIN
- Grant Writing Workshop-
- Dr. (Alan) Taylor Kelley has assisted with training UNHS staff on grant writing and assisted in the application of several grant funding opportunities focusing on behavioral health expansion. These grants were CCBHC, SBIRT, and N CREW.
- Funded: NCREW (Native Collective Research Effort to Enhance Wellness) is funded through NIH (National Institutes of Health) HEAL Initiative and are committed to support T/NASO (Tribal and Native American Serving Organizations) to lead community prioritized research projects. This is an exciting opportunity to build search infrastructure at UNHS. Read more about the ROA here
- Educational Brochures and Information- Brochures and posters that are culturally correct to aid those in the community that struggle with SUD
- Expanding Behavioral Health Resources- Expand services by improving recruitment and aiding current community members pass the Licensed Clinical Social Worker (LCSW) exam. So far, 3 individuals have passed and more are scheduled to try until August, 2025.
- EMS Training- EMS department looking to send 8 staff members to paramedic training (5 covered by RAIN).

St. John's Health
Accomplishments with RAIN
- Naloxone Pamphlet- Site is to make a Naloxone pamphlet that will be used in the pain clinic. This will help education and access to Naloxone in the hospital.
- Naltrexone Formulary Request- Request Naltrexone formulary from the pharmacy with evidence based literature.
- Drug Take Back Program- St. John's is to consolidate their take back efforts in the outpatient pharmacy including take back and drug disposing pouches.
- MOUD Care - Many providers received an x-waiver certification to expand addiction services.

RAIN Initiative
The project, the UUHRN-PARCKA Rural Addiction Implementation Network (RAIN Initiative), is a collaboration between the University of Utah Health Regional Network (UUHRN) and the University of Utah’s Program for Addiction Research, Clinical Care, Knowledge, and Advocacy (PARCKA).
MISSION: To improve access to care by implementing evidence-based addiction-related prevention, treatment, and recovery activities and services to reduce the morbidity and mortality of substance use disorder—including opioid use disorder—in high-risk rural communities, while improving the knowledge of addiction recovery, treatment, and recovery and implementation processes of rural health care practitioners.
To achieve this mission, over the course of three years, we will achieve the following aims:
AIM 1: “RAIN Teams” within four rural hospitals/health-systems of the UUHRN will implement and evaluate all the required evidence-based 5 addiction Prevention Core, 7 Treatment Core, and 3 Recovery Core Activities amongst four rural hospitals/health-systems of the UUHRN over 36 months.
AIM 2: Educate and provide skills of 1) evidence-based addiction prevention, treatment, and recovery and 2) implementation processes to RAIN Teams within four hospitals/health-systems of the UUHRN.
Through these two aims we will develop a sustainable, collaborative infrastructure through the RAIN Initiative where the consortium can be:
- Responsive to emerging addictions among their medically underserved patients
- Become a practice-based research network (PBRB)
- Disseminate the RAIN Initiative results
- Enhance the ability of our rural network collaboration efforts to confront other addiction, and non-addiction, health care challenges and disparities. While we are starting out with only four rural hospitals, over time we hope to expand the reach and implement these initiatives to a larger population in other rural hospitals/systems.
In 2023, the RCORP RSV (Reverse Site Visit) was held in conjunction with the NRHA's Rural Community Health Connections Summit, from July 11th-13th. Celebrating five years of RCORP, this collaborative event offered opportunities to connect with HRSA staff, federal partners, NRHA, and key rural partners and leaders in rural health.
The NRHA's official slogan for the conference: Your voice. Louder.
Two members of the RAIN team were sent to this conference to connect with RCORP support members. It was a highly valued experience, we look forward to future RCORP conferences.
In 2024, the RCORP RSV (Return Site Visit) was an invaluable experience closing in on the end of the Implementation 3 cohort. Speaking from lived experience and their work in addiction, Michael Botticelli and Judge Linda Davis, shared helpful insight and awareness of the impact stigma may have on rural communities.
Frequent breakout sessions allowed opportunities for collaborations with other RCORP grantees and sharing of resources/challenges throughout the last 3 years. Thank you RCORP!