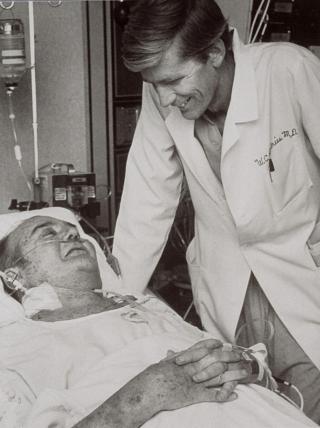
Dr. Lyle Joyce

Dr. Lyle Joyce has been practicing in the field of cardiothoracic surgery for more than 40 years, focusing on heart transplantation and the surgical treatment of heart failure. He is world-renowned in the field of cardiothoracic surgery having been on the team that implanted the first permanent artificial heart in a man, and was the first surgeon ever to use a total artificial heart in a woman.
When did you know that you wanted to study medicine?
I knew as a young child that I wanted to go to into this field. It was probably initiated by the experiences I had on the farm with my father. We had a diverse farm with cropland as well as animals (beef and dairy cattle, hogs, chickens, and a horse) and I grew up learning to farm with my dad. I loved working with him. Anytime an animal got sick and died, he would have the veterinarian help us conduct an autopsy to determine the cause of death. The medical aspect of farming excited me, but I knew I wanted to treat humans rather than animals. As I got interested in medicine, much of the news headlines were about the first attempts of doing open heart surgery using anything from a deep hypothermia, cross circulation, and eventually a heart lung machine.
Dr. Debakey became very popular with performing the first abdominal aneurysm repair using his hand sewn Dacron graft and many other “firsts”. It seemed in those days, everything was a race to be first – the arms race, the space race, and the race to be the first to do open heart surgery. I wore glasses and couldn’t be an astronaut so that left heart surgery as the best race for me to enter. As a sophomore in high school, my school superintendent suggested that a Nebraska farm boy attend a college that was a little closer to my hero’s (Dr. Michael Debakey) medical school. I attended Baylor University in Texas and during the summer break between my junior and senior year, I was selected for a research position in Dr. Debakey’s lab. After Medical School I spent 7 years at the University of Minnesota for General Surgery Residency. In July 1980 I started the CT Surgery Fellowship in the University of Utah. (see Dr. Joyce’s interview given to Dr. Jason Han)
What were some of the best memories you have from your training in Utah?
From a non-medical standpoint, skiing is my best memory. It was great to be able to walk out of the hospital after being on call and be on the slopes in 20 minutes. I had never skied before, but the university offered tuition free classes and Tina, my wife, took classes during the week and then she would teach what she learned to our children and me on the weekends. And, of course, La Caille! What a beautiful place! Everything about Utah has a warm spot in my heart. From a surgical training perspective, the University and LDS Hospital program really was exceptional. The rumor was at the time that residents were actually performing more cases in Utah than anywhere in the county. And the faculty was exceptional. Each faculty member was a little different and each brought a different style of teaching, but everyone made you feel like family.
Dr. Hal Liddle had room 13 in LDS Hospital OR and Dr. Russell Nelson had room 14. Each day, one resident was with Dr. Nelson and one with Dr. Liddle. Dr. Nelson was soft spoken and Dr. Liddle more of a traditional teacher, very demanding, very high strung. The residents joked that room 13 had a tremor virus because we felt a little more pressured. Both aspects were good to train a new surgeon. Both made me feel like I could be their son, and I would think that they were taking a special interest in me. But the other residents felt the same way. That meant they were treating all the residents to feel they could be the best they could be. Their families would often the residents to their houses often so it was easy to feel special and wanted.
What were some of the best lessons you have learned in your career?
I learned what it was like to be a pioneer under the scrutiny of the highly publicized experiences with Barney Clark. Sometimes it seems like it was yesterday. The excitement of being a part of a new break through spurred me to continue to stay in the field. Something that I’ve learned over the years is the importance of the team. You can’t get anything done, other than routine things, if you don’t have a team behind you. That means keeping that enthusiasm and making it contagious so other people can share the excitement. Another lesson that I learned is that you are only as good of a surgeon as your first assistant. When I left Utah, I went to a non-academic setting and we didn’t have residents. It didn’t take me long to find the best scrub nurse available (at that time we didn’t have PAs or NPs) and I taught to be a star assistant. It is like conducting an orchestra. Another lesson learned is that we must always strive to do our best, but the ultimate outcome is in God’s hands!
What have you been up to since your time in Utah?
After the Jarvik 7/TAH implant of Barney Clark, Dr. DeVries and I knew it was going to take a long time to do the second implant at Utah. I moved to Minnesota to start the artificial heart program there and Bill went to Louisville. I started the Artificial Heart and Transplant Program at the Heart Institute and was also volunteering at the University with their program where I was interim chief for 3 years. As a private group we were operating in multiple different hospitals. During that time, my daughter, Dr. Sheri Crow, had attended Medical School and finished her training in Pediatrics and Pediatric Critical care at the University of Minnesota. She was then hired at the Mayo Clinic. When a Cardiovascular position became available at the Mayo Clinic, my wife suggested I would be crazy not to take that opportunity. So, we moved to follow the grandkids. At Mayo, my youngest son, Daniel (now a Urologist) was in medical school and my oldest son David was hired as a CT Surgeon as well and his wife Joyce joined the Infectious Disease faculty.
For a period, there were 5 Joyces practicing medicine at the Mayo Clinic. 5 years ago, David and I moved to the Medical College of Wisconsin to build their VAD and transplant program. Their residency program was on hold due to low surgical volume. After joining, we received CMS approval in 6 months and have been growing and now have 8 surgeons on staff. My real love has always been teaching. We’ve always been interested in international work. Kenya has been the latest program we have developed. We started a Cardiothoracic residency program based on the US STS Core Curriculum, so the trainees get the same didactic teaching as the US residents. There are online classes and surgeons from Canada and the US rotate to Kenya for hands-on teaching. I go twice a year. There were no other Sub-Saharan cardiac training programs between Cairo, Egypt and Johannesburg, South Africa. It has been highly successful and they are now able to do 3 – 4 heart surgeries a week on their own with the visiting teams focusing on teaching highly complex cases.