Novel Electronic Preoperative Screening Tool to Guide Appropriateness for Ambulatory Surgery
Introduction: Ambulatory surgery is becoming increasingly common, yet the selection of patients who are appropriate for ambulatory surgery remains challenging. Factors that place patients at higher risk for complications in an ambulatory setting are often unclear to or unrecognized by surgeons and/or their schedulers. When patients are scheduled for surgery at an ambulatory surgery center (ASC) and subsequently deemed an inappropriate candidate on the day of or day prior to surgery, it justly may create frustration for the patient, surgeon, and surgical facility leading to added stress for the patient and potential loss of revenue for the hospital system. In order to address this issue and automate part of the screening process, we created an electronic preoperative screening tool to help capture patients early on in the scheduling process who may be inappropriate for ambulatory surgery. The tool captures certain diagnoses, physical characteristics, and surgery variables in order to flag the patient for a preoperative review by an anesthesiologist in advance of their scheduled surgery. Our goal, through implementation of this tool, was to prevent same-day or day-prior cancellations.
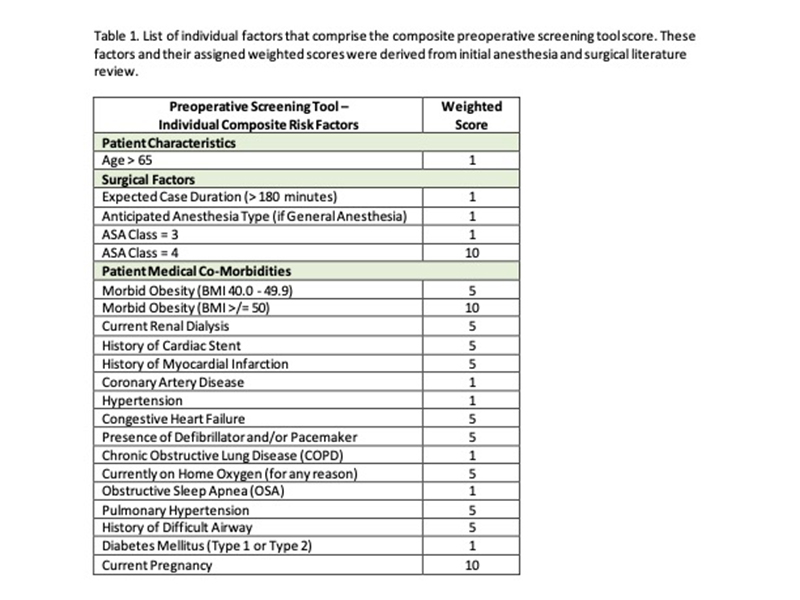
Methods: Through a review of current literature, surgical factors and patient comorbidities associated with increased morbidity, mortality, or hospital admission after surgery were identified and assigned a score between 1-10 based on relative risk. An automated computer program was created to mine the electronic health record for these comorbidities, calculate a score, and aggregate the scores to a spreadsheet accessible to scheduling staff. Approximately 1-2 weeks prior to proceeding with ambulatory surgery, patients at elevated risk were identified using our tool and were forwarded for further review and approval by an attending anesthesiologist. Initial screening tool implementation and the corresponding anesthesiologist review process was conducted over a one month period from 2/4/21 through 3/5/21 at a single university ASC site.
Results: There were 122 total surgical cases. With applied predetermined threshold scores, the screening tool identified 16 total patients as either increased or high risk, representing 13% of all scheduled patients. Of these, 9 (56%) were scheduled for general anesthesia and 10 (62.5%) had a BMI above 40. The average composite risk score in this group was 13.7, compared to 3.3 overall. Altogether average ASA score was 2.4 and is included in the composite risk score (if ASA >/= 3) but requires a historical anesthesia evaluation of which only 42 (34%) had documented. Of the identified increased risk patients, 5 (31%) did not require anesthesia review (most often due to low-risk anesthesia type such as topical and/or a low-risk surgical procedure such as cataract removal and 7 (44%) were correctly flagged by pre-operative nursing staff to request further anesthesia review prior to the day of scheduled surgery. Of the completed reviews, these were done on average 4.6 days prior to scheduled surgical date and there were zero same-day case cancellations or changes during the initial implementation month.
Conclusions: This study is among the first to demonstrate an automated screening tool working jointly with the electronic health record to guide ASC patient selection. Implementation across multiple ASC locations and increased surgical case volume will allow further modification and validation creating a reliable tool for efficient ASC scheduling.