 |
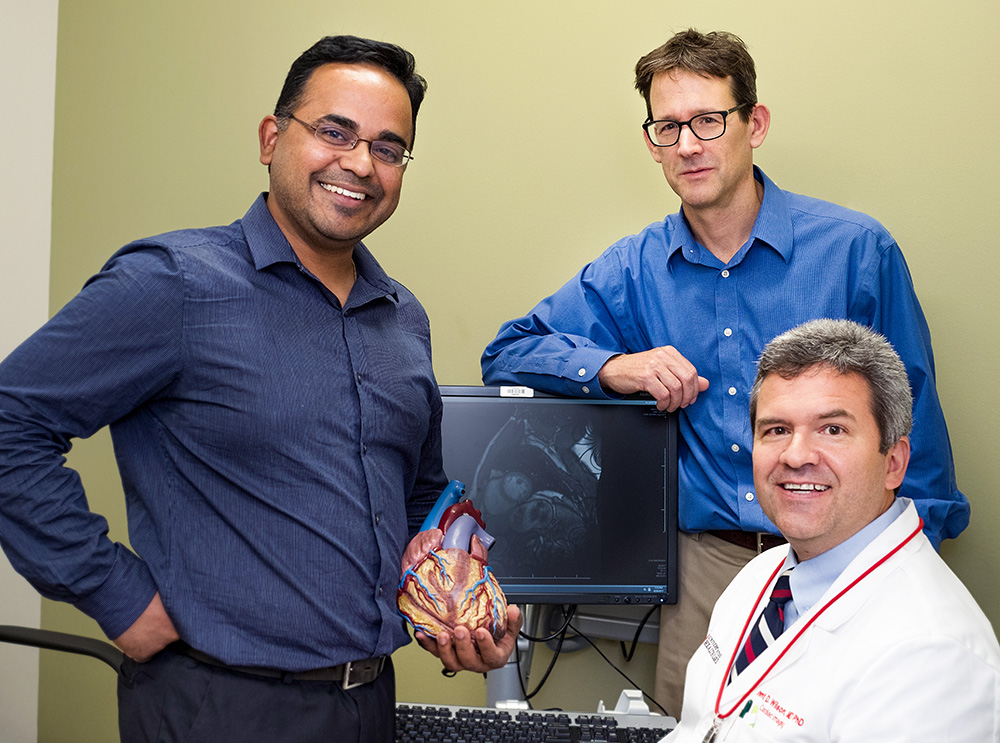
| Collaborating researchers (left-to-right): Ganesh Adluru, PhD (Radiology and Imaging Sciences), Ed DiBella, PhD (Radiology and Imaging Sciences), Brent Wilson, MD, PhD (Division of Cardiology). |
By Michael Mozdy
With 1 in 4 of all American deaths coming from heart disease, having a good way to diagnose and direct treatments is a big deal. For suspected heart problems, cardiologists have a number of non-invasive tests to help them see what’s happening. Each, however, has its drawbacks.
Ganesh Adluru, PhD, a faculty member in the Department of Radiology and Imaging Sciences, has been developing new MRI techniques that promise to significantly advance how physicians identify coronary heart disease (the most common form of heart disease where blood vessels become clogged with plaque).
For quite some time, a nuclear medicine test called SPECT myocardial perfusion imaging has been the go-to test to diagnose coronary heart disease. SPECT has been a valuable tool to help cardiologists identify where they should consider treating blood vessels with angioplasty, stents, or bypass surgery. The SPECT test is relatively easy to perform but is not always accurate. It is also limited in three other ways: 1) it produces blurry images due to “noise” inherent in the nuclear medicine scan as well as heart motion, 2) it takes about 3 hours for a patient to complete the exam, and 3) patients are exposed to some radiation in the nuclear tracers that are used.
One alternative to SPECT is a computerized tomography (CT) angiogram with injected iodine contrast dye. While SPECT is aimed at heart muscle tissue, CT angiograms produce images of the coronary blood vessels to find out if they appear to be blocked. The CT angiogram has the advantage of only taking 5 minutes to accomplish and it produces beautiful, accurate pictures of vessels in and around the heart. But blocked arteries don’t necessarily mean diseased heart tissue – many patients with small blockages can continue a long and healthy life with vigorous exercise. CT angiograms also subject patients to radiation.
Adluru and his colleagues specialize in magnetic resonance imaging (MRI), which does not use radiation. Like SPECT, the MR scan looks at perfusion, or blood flow, within heart tissue. The MR scan does not use radiation, but does use a “contrast agent” that is injected and helps the areas with blood flow appear more clearly. The trick with MR perfusion is that once the patient’s heart rate is high enough (called being “at stress”), there is a window of about 30 seconds to best capture images of the contrast agent is being taken up in the heart tissue. Until recently, MR scans were simply too slow to capture the uptake in all (or even most) of the heart muscle during the crucial 30-second window. Recent advances in MRI have drastically changed the playing field, however, and Adluru is on his way to developing a quicker and more accurate MRI test for cardiac perfusion.
Building a Faster, More Complete MRI Scan
When an MRI scanner collects data from a patient, it’s not like taking a picture with a camera. The scanner manipulates magnetic fields around the patient and captures how protons in the body line up along these fields. The data takes the form of numbers in a complex matrix. If you printed it out, it would look like a thousand scattered dots, and nothing like the human anatomy sitting inside the scanner.
 |
| Ganesh Adluru, PhD, faculty member in the Department of Radiology and Imaging Sciences and researcher at the Utah Center for Advanced Imaging Research (UCAIR). |
The process of converting this electrical/magnetic data into an image that radiologists can recognize is called image reconstruction. Adluru works in the Department’s think tank for imaging innovation: the Utah Center for Advanced Imaging Research (UCAIR). He came to UCAIR in 2004 as a PhD student and has been working with Ed DiBella, PhD, the current UCAIR Director, on cardiac MR perfusion studies since then. They specialize in the complicated math and techniques needed for advanced image reconstruction.
Adluru came into the field when researchers were concentrating on making the scanning and image reconstruction phases quicker. Based on the theory that a lot of the information gathered was redundant, researchers only acquire a portion of the data (called undersampling). With this technique, they are able to perform an 8mm MRI cross-section, or “slice,” in 60 milliseconds rather than 250 milliseconds. In the case of a moving target like the heart, this 4-fold decrease in time of scanning makes a big difference.
As part of the NIH-funded Human Connectome Project, several labs developed another new MRI method, called simultaneous multi-slice (SMS) imaging. Using a novel technique to excite the body’s protons in multiple places at once, SMS allows researchers to collect data on 3 different slices over the same amount of time they would normally collect just one slice.
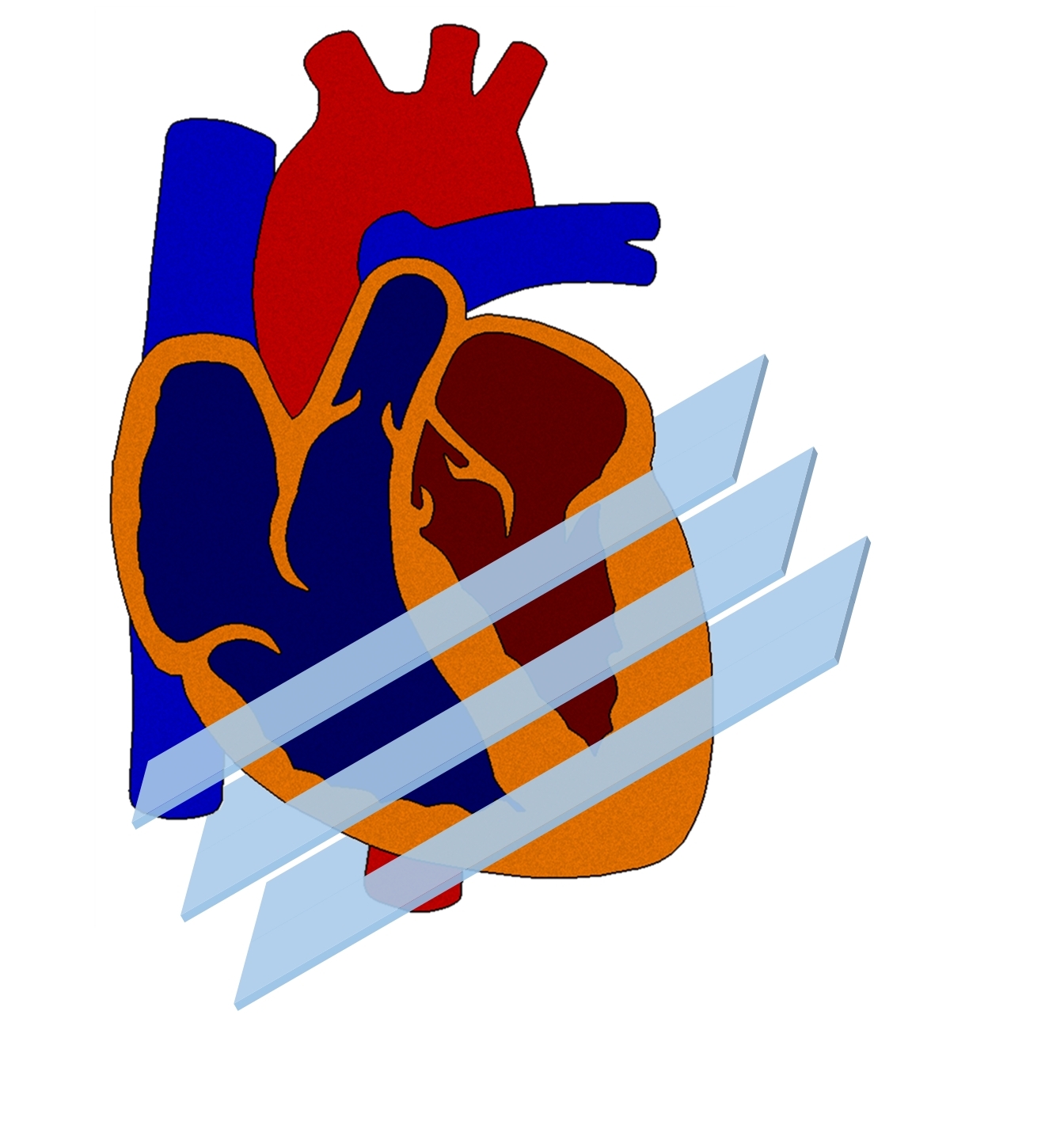 |
| An illustration of how the SMS MRI technique captures three cross sections of heart tissue at the same time. |
“It’s like shooting an arrow at an apple in a tree,” illustrates Adluru. “Instead of just shooting one arrow, we’re able to pull back the string on the bow and release three arrows at once.”
Adluru and DiBella were exploring these kind of methods in a brain imaging study at Utah when Adluru had a hunch that they could be adapted for cardiac imaging. He believed they could be applied alongside the fast undersamping methods to garner even greater efficiencies.
SMS provides compressed data that needs more computational power, but the gain in coverage over the heart is well worth it. Standard undersampling collects four 8mm-thick slices in 250 milliseconds, but misses 17mm of heart tissue in between each slice. By combining undersampling with SMS, Adluru and his collaborators achieve the quick scan time with three times as much coverage. They can collect twelve slices in the same amount of time with essentially zero gap in between slices. This more robust data set makes any diagnosis much more reliable.
Putting Fast-Acquired SMS to the Test
In March 2017, Adluru received word from the NIH that his 4-year grant application for his proposed work exploring SMS cardiac MRI was funded. This was amazing news for a young faculty member on his first try for the flagship of NIH grants, called the R01.
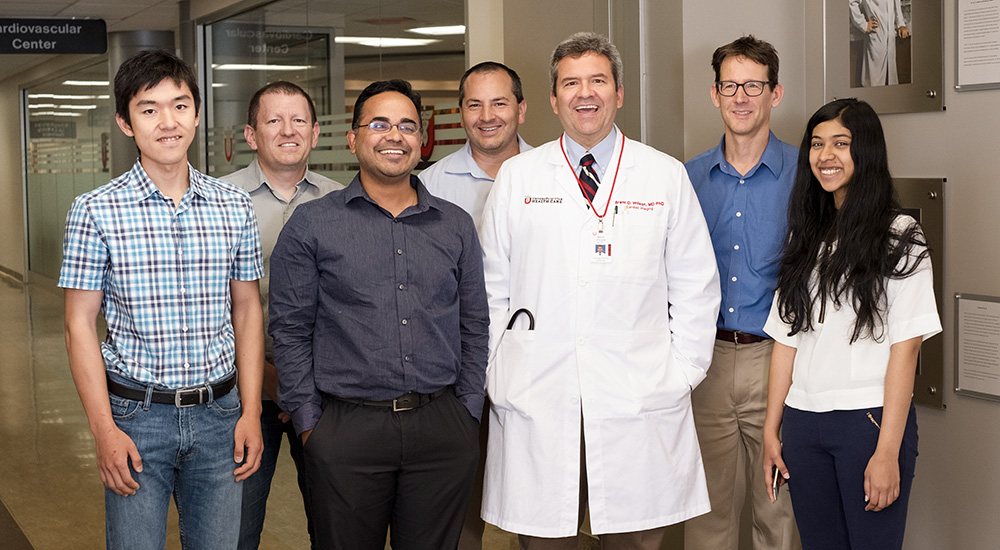 Adluru’s collaborative team (left-to-right): Ye Tian (graduate student), John Roberts, PhD, Ganesh Adluru, PhD, Jason Mendes, PhD, Brent Wilson, MD, PhD, Ed DiBella, PhD, Apoorva Pedgaonkar (graduate student)
Adluru’s collaborative team (left-to-right): Ye Tian (graduate student), John Roberts, PhD, Ganesh Adluru, PhD, Jason Mendes, PhD, Brent Wilson, MD, PhD, Ed DiBella, PhD, Apoorva Pedgaonkar (graduate student)
“It’s exciting to watch him develop over the years,” praises DiBella, “And – wow! – on his first try he gets an R01 funded.”
Part of Adluru’s success can be attributed to the great track record he and DiBella’s team have established in image reconstruction techniques; part is due to Adluru’s innovative combination of techniques, especially as applied to cardiac MRI, where he is one of the first to be using SMS. And much is also due to his strong partnerships with clinicians at the University of Utah Cardiovascular Center.
The primary clinical collaborator for Adluru’s grant is Brent Wilson, MD, PhD, a faculty member in the Division of Cardiology and adjunct faculty in Radiology and Imaging Sciences. As a practicing cardiologist, Wilson will recruit patients to the study, and he will read and interpret the cardiac images provided by Adluru.
The mini-movies that Adluru puts together show how blood moves through cross-sections of the heart. If there is good blood flow through the tissue, the white contrast agent moves quickly through that portion of tissue. When tissue lacks strong blood flow (such as when the blood vessels feeding it are obstructed with plaque), the tissue appears darker because less contrast agent is moved through them. Wilson’s job is to analyze the light and dark spots – pixel by pixel when necessary – to identify problem areas in the heart.
An example of the SMS cardiac perfusion study - the slices of the heart start in the upper left (top of heart), progress left-to-right, then to the middle row (left-to-right), and then the bottom row, with the lower right corner showing the bottom of the heart. Midway through the video, you can see the white contrast enter the heart tissue, which shows blood flow, or perfusion. Video courtesy Ganesh Adluru, PhD.
Wilson is excited about the accuracy provided by Adluru’s reconstruction methods. “Our hypothesis is that we can show that this safe, quick MRI scan is a great tool for diagnosing coronary artery disease and determining who should consider more invasive treatments to fix their disease,” he explains.
Adluru is optimistic about the usefulness of his method beyond diagnosing coronary artery disease. “This scan can be a great way to track the effectiveness of treatments,” he declares. “It can show whether a stent or angioplasty restored enough blood flow to rescue the suffering cardiac tissue.” In other words, these scans could provide a critical 6-month or 12-month follow-up to assess a patient’s heart health after treatments.
Researchers and cardiologists have spent decades exploring a range of technologies to help diagnose, treat, and monitor the body’s workhorse organ. We still have a way to go, but thanks to Adluru, we have a quick and more complete MRI perfusion scan in development. Our team in the Department of Radiology and Imaging Sciences is proud to be at the front lines of this quest to provide the best medical approaches for one of the biggest killers of our time, heart disease.