By Michael Mozdy
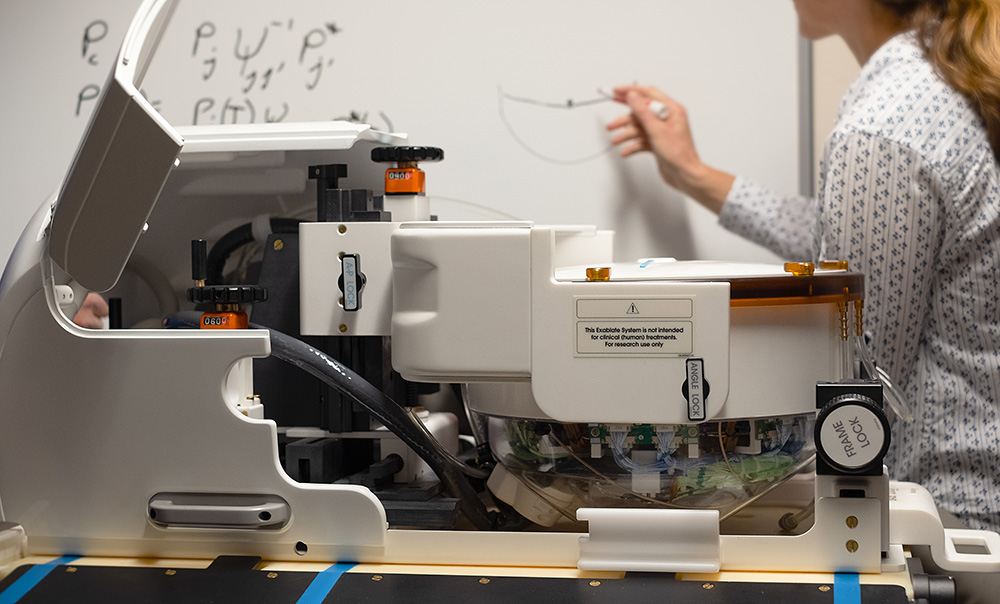
In August 2018, researchers at the Utah Center for Advanced Imaging Research (UCAIR) excitedly unpacked a carefully shipped piece of technology. It was a sophisticated-looking dome of a helmet, meant to fit a patient’s head and be used in an MRI machine, dubbed with the futuristic name “Exablate Neuro.” It was the fruit of months-long negotiations and partnership with the manufacturer, InsighTec, a pioneer in MRI-guided focused ultrasound applications for the brain.
UCAIR is home to experts in this exact technology: Dennis Parker, PhD, Allison Payne, PhD, Rock Hadley, PhD, Viola Rieke, PhD, and a host of research associates, engineers, and graduate students. Part of the reason the manufacturer was happy to enter this partnership with the University of Utah was because our Department of Radiology and Imaging Sciences researchers would continue to advance the precision, effectiveness, and safety of treatments with the Exablate Neuro. InsighTec engineers were on hand to help set up and test the device, and remain in close contact with our researchers.
In late January 2019, the University of Utah will be the only site in the intermountain region to offer this noninvasive, FDA-approved treatment for essential tremor. This milestone is actually even more significant: we’re the first site in the USA to use the Exablate Neuro on Siemens MRI machines, and the only site between Stanford to the West and Mayo Clinic to the East to offer the treatment.
But our researchers see this as just the beginning of how focused ultrasound might be used for neurological conditions. They’re already hard at work attempting to usher in the next generation of applications.
Challenges in the Cranium
 |
 |
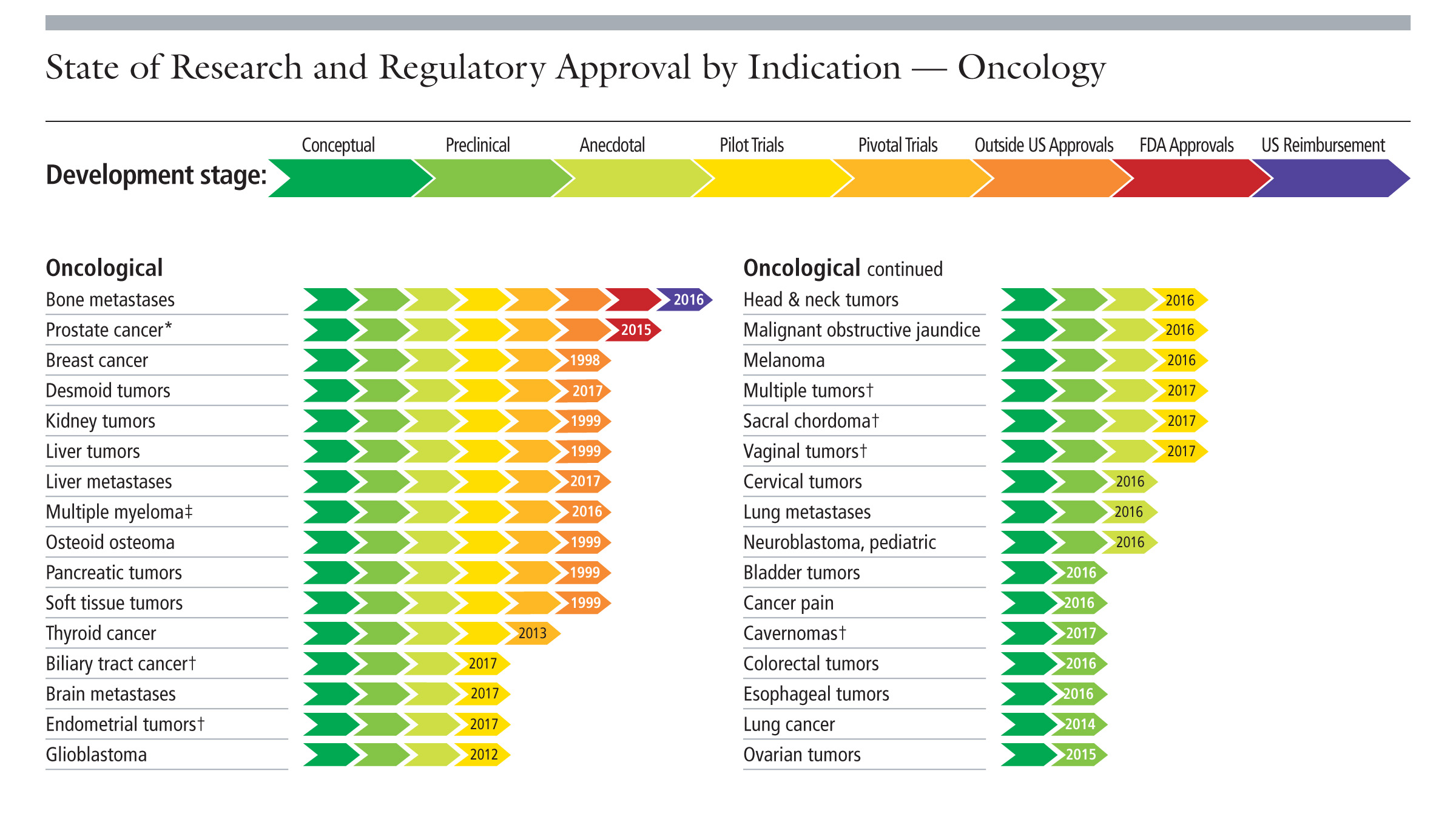 |
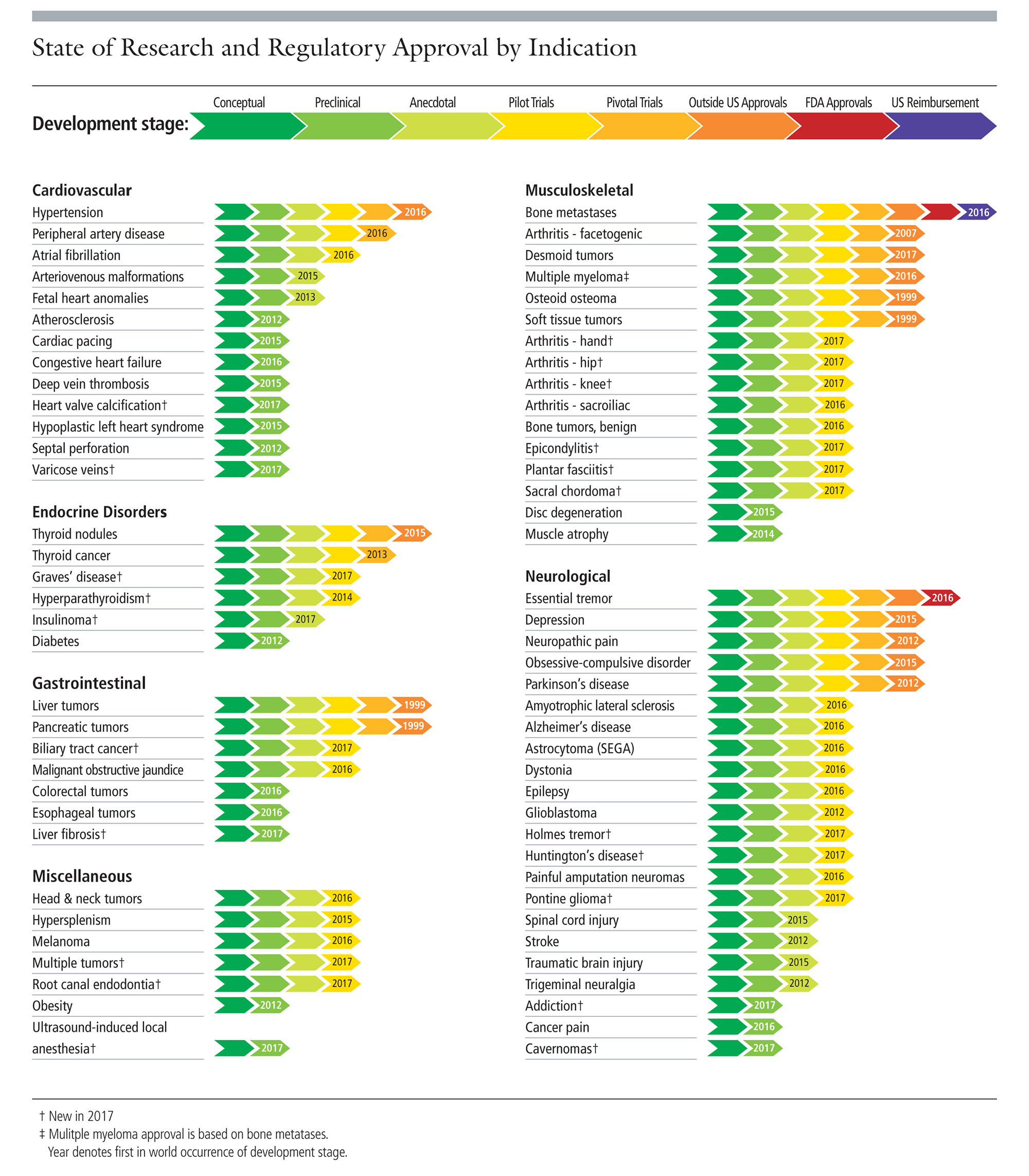
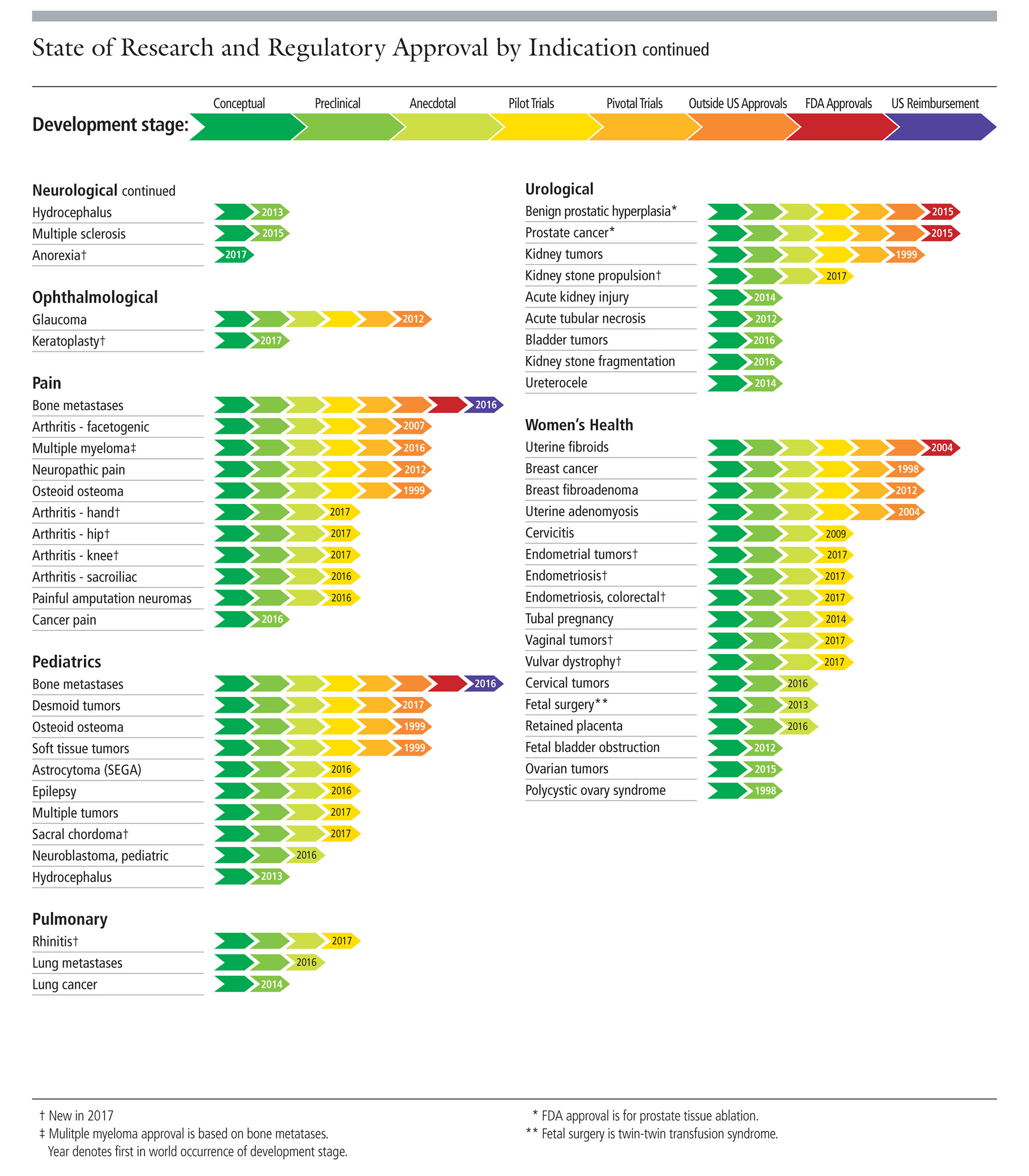
| Charts from the Focused Ultrasound Foundation. |
High-intensity Focused Ultrasound (HIFU) treatments have been FDA approved for different pathologies for some time – the first was uterine fibroids in 2004. The charts here provide the timeline of this noninvasive technique in treating a huge array of conditions (click on each for a closer look). In fact, Payne and Parker are currently pursing clinical trials for their first-in-class Muse system to treat breast tumors.
But using HIFU in the brain is a tricky business. It boils down to the fact that a millimeter in any direction might impact something very different than the intended target. Since HIFU operates by focusing high-intensity sound waves to a point some distance away from the device that creates the waves (called the transducer), those sound waves need to travel across tissue and bone to reach their intended target. Yet no cranium is identical: there are obvious differences in size and shape, but also the thickness of a person’s cranium varies from top to bottom and side to side. Sound waves get minutely re-directed when they travel through bone as opposed to soft tissue. This means that to achieve an accurate application of HIFU to a brain region, lots of mathematical modeling and a clear mapping of each patient’s brain must take place.
InsighTec’s Exablate Neuro system has risen to the challenge. It can accurately place HIFU in the tiny region responsible for essential tremor with immediate results.
UCAIR researchers, led by Parker, are looking to improve upon the system in a number of ways.
Volumetric 3D Temperature Mapping
HIFU heats up and “cooks” the tissue where it is focused. In the case of treating essential tremor, this damages the portion of the brain responsible for the tremor, without the need for more risky cranial surgery. The key to doing this safely is to monitor the temperature of the tissue and know when you’ve delivered enough energy but not too much. Excessive energy might overcook or even boil soft tissue – which can transfer heat to surrounding tissue and cause excessive swelling or edema. Thanks to advances in MRI science, clinicians can now measure temperature noninvasively with MRI (much better than sticking temperature probes into the brain, which essentially defeat the purpose of noninvasive treatments). Parker, in fact, was the first scientist to publish a way to measure temperature with MRI, back in the 1980s.
Yet clinical systems like the Exablate Neuro currently measure temperature along a single slice or plane (2D temperature monitoring). Scientists need to measure temperature as it changes in real time, but they must struggle with the time it takes to acquire an MRI image with magnetic pulses as well as the time it takes to work with the massive amount of data that they are given and make a sensible picture of temperature changes. Until now, the only practical way to do this in near-real-time was along a single plane. But walking around a campfire tells us that heat radiates in three dimensions, so it would be much more helpful to clinicians if they could have 3D, volumetric heat maps.
Parker and his team are well on their way to solving this issue. “3D temperature mapping has been around for about a decade,” he says, “and we’re down to about 1 image every 6 seconds.” They accomplish this with more involved pulse sequences – the sequence of magnetic pulses emitted by the MRI machine, which excite the protons in the water molecules in our body, allowing the electromagnetic signals captured to tell the tale of what our tissue looks like – as well as more advanced and quicker methods of reconstructing the signals that are captured.
The UCAIR group is not the only team hot on the trail of full volumetric MR temperature mapping. “We’re in a sort of gentleman’s race with Stanford, Vanderbilt and UVA,” Parker chuckles. “They’re all great people,” he adds. “We couldn’t have a nicer group of people to compete against, we’re all very good friends.”
Custom MRI Coils for the Exablate Neuro
Another strength at UCAIR is the Custom Coil Lab, with Hadley at the helm. They specialize in making custom MRI “receive coils,” which are the technology that reads the change in electromagnetic signal measured in the body after the MR pulse sequences are applied. All MRI machines come with receive coils built into the large bore of the device. But the inflexible laws of physics state that the signal will become fainter the farther away from the source you are. In other words, if you want to measure stronger signals and have less noise, you should put your receive coils as close to the body as possible.
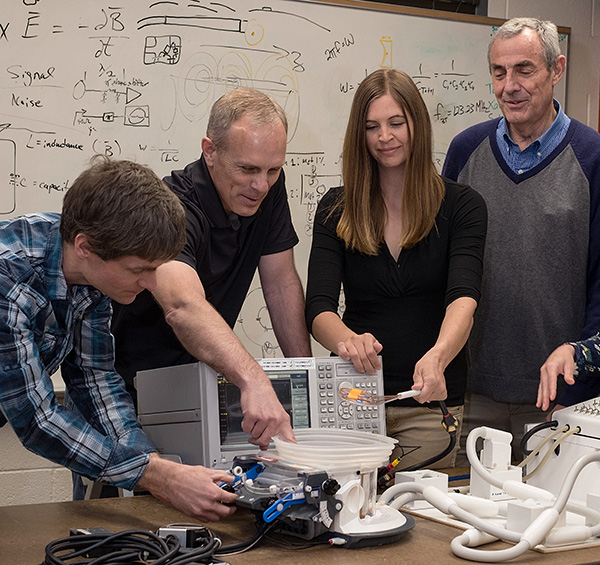 |
| Coil Lab members (right to left): Robb Merrill, Rock Hadley, Emilee Minalga, Dennis Parker. |
MRI manufacturers offer head coils and other body part coils to get closer to the body part being measured, but these one-size-fits-all devices are manufactured to take a lot of abuse in the clinical environment, and often sacrifice some resolution in the engineering compromise.
This is where our Coil Lab jumps in. They are masters at crafting custom, innovative MR coils – neck coils to better measure carotid artery plaques, head coils, calf coils, and breast HIFU coils, to name a few. The Exablate Neuro system provides an even more interesting challenge. First, the coils must interface with the hardware and programming of the InsighTec system as well as the Siemens MRI machine. Second, HIFU is accomplished through water since ultrasound travels much better through water than air. This means that a water barrier “couples” the transducer to the patient’s shaved head. Custom head coils need to operate in this water environment and not get in the way of the transducer that sends the focused ultrasound waves.
Elastography to Measure Tissue Changes
 |
| Lorne Hofstetter |
Measuring temperature is one patient safety and treatment efficacy metric, but another is to take a look at the physical changes happening in the tissue. If you’ve ever cooked a burger, you know what happens when the soft, uncooked meat barely holding its shape is flame broiled – it firms up, it releases fat and water, it shrinks, and parts that are closest to the heat source can even get hard to the point of being crispy. Physicians clearly have different objectives than we do at the BBQ, but these same principles apply when heating human tissue. Knowing that the tissue was raised 20 degrees Celsius doesn’t tell you much about the physical properties of that tissue.
A PhD-MD candidate in Parker’s lab, Lorne Hofstetter, has made a breakthrough this past year in helping to noninvasively visualize physical changes with a technique called MR elastography. Hofstetter’s work helps clinicians see how tissue changes in its stiffness or “spring.” When combined with MR temperature mapping, it creates a multi-parametric way to measure effectiveness of the treatment and to ensure the safety of the patient.
HIFU Histotripsy in the Brain
In addition to ablation, where long pulses of intense ultrasound are applied to tissue in order to heat it, HIFU can do more. Histotripsy is a technique that fascinates Parker and his clinical partner, Matthew Alexander, MD, and John Rolston, MD, PhD. Histotripsy uses HIFU to generate a mechanical effect on tissue instead of heat.
Parker explains that histotripsy involves very intense and “very, very short” ultrasound pulses that hit an area of tissue and cause extreme changes in pressure. Dissolved gases and water vapor come out of solution, a process called cavitation. The tissue essentially vaporizes.
“Many people are concerned about accuracy,” notes Parker. “Whatever you hit will be gone.” Perhaps for this very reason, “nobody has done histotripsy in the cranium,” he adds.
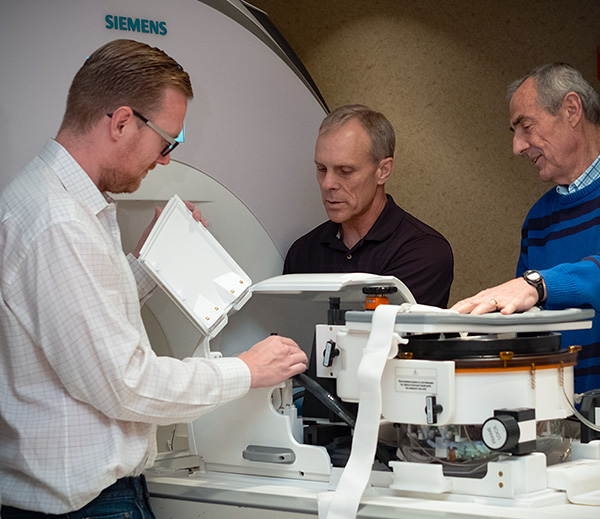 |
| Matthew Alexander, Rock Hadley, and Dennis Parker look “under the hood” of the Exablate Neuro. |
Yet Alexander and Rolston see a huge opportunity for applying this type of vaporizing treatment in the brain. “Histotripsy could dramatically improve options for patients with different diseases,” says Alexander, a neurointerventional surgeon.
Rolston, a functional neurosurgeon, explains, “for many neurological disorders there is no treatment outside of removing part of the skull to excise diseased tissue.” HIFU histotripsy might provide a noninvasive way to remove useless tissue by vaporizing it.
Parker, Alexander, and Rolston are investigating the Exablate Neuro’s ability to deliver slightly less intense, slightly longer (but still quite short) pulses to tissue in a novel histotripsy technique that has not been performed in the brain before. The experiments are a long way off from clinical applications in humans, but it demonstrates the great potential that HIFU and a system like the Exablate Neuro have for the future of neurological treatments.
“MR-guided HIFU is really a game changer for medicine, especially in procedural fields constantly looking to reduce invasiveness,” declares Alexander. “Brain surgeries always carry the risk of infection and other unintended complications. The advent of truly noninvasive treatments allows us to keep the skull and its contents intact while treating patients.”
The University of Utah and UCAIR are proud to be on the cutting edge of techniques that improve medicine and the quality of the patient experience. We look forward to seeing advances in MR-guided HIFU in the near future.